Krishnendu Roy was very familiar with the news coming out of Philadelphia, about the progress of clinical studies assessing an experimental treatment for leukemia, developed with Novartis Pharmaceuticals by University of Pennsylvania researchers. He knew all about Emily Whitehead, the young girl who was the first patient to test the first engineered cell therapy in history.
Emily’s leukemia is still in remission five years after undergoing a 2012 clinical trial at Children’s Hospital of Philadelphia of the groundbreaking drug by Novartis, Kymriah (tisagenlecleuce). In a global trial, 83 percent of terminally-ill patients went into complete remission. In August of this year, Emily and her family celebrated the U.S. Food and Drug Administration’s (FDA) approval of the revolutionary T-cell therapy for acute lymphocytic leukemia, the world’s first genetically engineered immune therapy.
It’s the kind of epic story that reminds Roy, a researcher at the Petit Institute for Bioengineering and Bioscience at the Georgia Institution of Technology, why he does what he does.
“These patients, like Emily, are incredibly brave,” says Roy, who holds the Robert Milton Chair in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory University. “They face the unknown – these potentially risky, potentially promising therapies. At the end of the day, it is for them, for the patients. I think everybody who works in the cellular therapies space, works with that motivation in mind.”
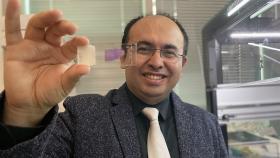
Over the past few years, Roy has taken the lead role in expanding that space at Georgia Tech, where he is director of the Center for ImmunoEngineering, the Marcus Center for Cell-Therapy Characterization and Manufacturing (MC3M), and the recently-established National Science Foundation Engineering Research Center for Cell Manufacturing Technologies (CMaT).
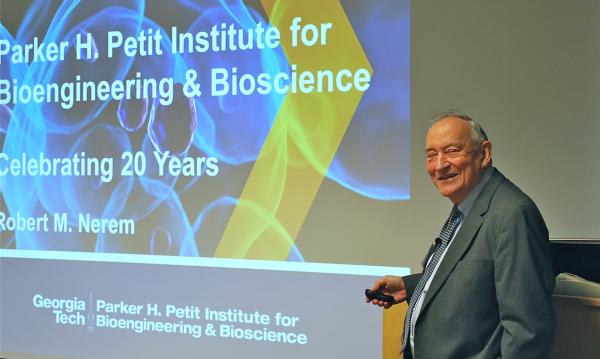
Roy is running point in a widespread endeavor at Georgia Tech to develop cutting-edge cell therapies, and CMaT, which launched this fall, is the latest highlight in a surge of cell therapy-related activity that goes back to the early 1990s, “when we went after a Whitaker Foundation development award and decided the focus should be on tissue engineering – the engineering of replacement tissues using living cells,” notes Bob Nerem, founding director of the Petit Institute.
“We got that award and began our initiative with three initial focus areas,” Nerem adds. “The cardiovascular area, diabetes, and orthopaedic tissue engineering. Later, we added the neural area, which in many ways has to be considered the holy grail, because there aren’t any viable treatments for many neural issues.”
And that’s the point of cell therapies: they offer a powerful alternative to patients with a dwindling supply of hope.
“We believe cell-based therapies can provide new treatment options," Nerem says. "We feel that’s the future, and we hope to make a major contribution for patients who are running out of options."
Collaborative Heft
In September 2017, the National Science Foundation (NSF) announced it was awarding $20 million to a Georgia Tech-led consortium of universities to establish CMaT, which will serve as the catalyst for a new epoch in the evolution of cell therapies. CMaT researchers will collaborate with industry and clinical partners to develop tools and technologies for the consistent, scalable, and affordable production of living therapeutic cells, which could be used to battle cancer, heart disease, autoimmune diseases, and other disorders.
Almost 20 years earlier, NSF sparked cell therapy research with a $12.5 award to establish GTEC – the Georgia Tech/Emory Center for the Engineering of Living Tissues.
“Georgia Tech has been showing great leadership in cell therapy research for a number of years,” says Bob Guldberg, executive director of the Petit Institute and professor in the Woodruff School of Mechanical Engineering. “GTEC really helped build a critical mass of people here doing regenerative medicine research and established Georgia Tech as a national leader in tissue engineering and regenerative medicine.”
GTEC has since evolved into the Regenerative Engineering and Medicine (REM) research center, a collaboration of Tech, Emory University, and the University of Georgia (UGA).
With CMaT, the number of collaborators has grown. In addition to Georgia Tech, major partners include UGA, the University of Wisconsin-Madison, and the University of Puerto Rico (Mayaguez campus), as well as affiliate partners Emory, the Gladstone Institutes, Michigan Technological University, and the University of Pennsylvania.
A collaboration across many disciplines is going to be necessary to tackle the complex challenge of properly manufacturing cell therapies. Georgia Tech seems well-poised to lead such an effort, because of its own multidisciplinary capacity.
“Now we need a broad group of stakeholders to come into play, not only the clinicians and the biomedical and chemical engineers that have traditionally dominated the field,” says Roy, who led the National Cell Manufacturing Consortium – a collaboration of more than 25 companies and 15 academic institutions, along with government agencies and private foundations, that produced a national roadmap for large-scale cell therapy manufacturing.
“We’re bringing in electrical engineers, mechanical engineers, industrial engineers, basic scientists, as well as automation and robotics personnel and experts, data scientists, computational scientists,” Roy adds. “Bring all of that together with policy experts and our natural science programs, and it makes an ideal coalition. That crosstalk between so many disciplines at Georgia Tech makes it an ideal place for an effort like CMaT.”
Tech Marks the Spot
In the spring of 2014, the National Institute of Standards and Technology (NIST) awarded a $500,000 advanced technology planning grant to Georgia Tech, funds specifically allotted for creating a national roadmap and consortium targeting cell manufacturing. The NCMC emerged from that, under the direction of Georgia Tech and the Georgia Research Alliance (GRA).
In June 2016 at the White House Organ Summit, the consortium presented its 10-year plan, Technology Roadmap 2025, that basically details the critical stages in the manufacturing pipeline, including cell processing, cell preservation, distribution and handling, quality control, standardization, and workforce development.
Six months before the roadmap’s public unveiling, Georgia Tech was already on the right path. In January 2016, The Marcus Foundation awarded Tech $15.7 million to build a new research center for the development of processes and techniques to ensure the consistent, low-cost, large-scale manufacture of high-quality cells to be used in cell therapies. With additional funding from the GRA and Tech, the $23 million MC3M – the first research facility of its kind – was launched.
“The Marcus Center is already serving as a cell characterization hub for a network of clinical trials around the country,” says Guldberg. “This is a tremendously exciting role, because Georgia Tech will have a lot of the data that will be used to correlate what the important attributes of a cell are that determine whether it’s going to work clinically.”
Initial funding for the MC3M was slated for five years, after which time the center would be expected to support itself with corporate, government, and nonprofit funding. So, through MC3M, Georgia Tech (in partnership with institutions around the state and country) applied for federal funding from NSF to further augment its research and development in cell manufacturing.
With a strategic roadmapping plan in place and funding for a unique cell manufacturing and characterization center secured, Georgia Tech was well positioned to apply for one of the highly competitive NSF Engineering Research Centers. From an initial group of more than 170 proposals nationwide, CMaT was selected as one of just four newly funded centers for 2017. CMaT is headquartered in the Petit Institute for Bioengineering and Bioscience and will focus on developing enabling technologies as well as the workforce needed by the emerging cell manufacturing industry.
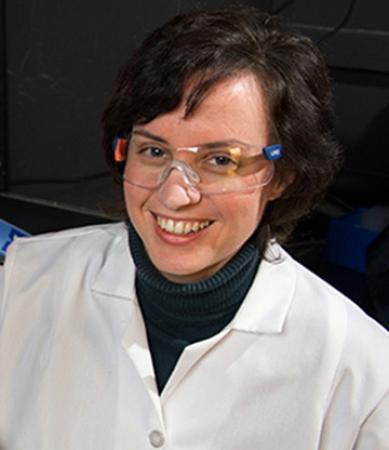
“I think we’re at a critical juncture in cell manufacturing,” says Johnna Temenoff, Petit Institute researcher, professor in the Coulter Department, and deputy director of CMaT.
“If we do this right, there’s a huge potential,” adds Temenoff, co-director of REM. “The long term goal is to have a large pool of high-quality cells that we can get to people around the world in developed and developing countries.”
This idea of creating affordable new-age medicine for a global population is a major goal for cell therapy and manufacturing researchers like Roy, who notes the high cost of cell therapies. The pioneering Novartis T-cell therapy that cured Emily Whitehead’s cancer is listed at $475,000.
“These treatments can be very expensive, and inaccessible to a majority of the people in the world,” Roy says. “So, the burning question is, how do we bring this to scale and make these therapies cost-effective and available for a broad population across the world, regardless of socioeconomic status? As long as we can develop reproducible product at a much lower cost and achieve manufacturing that is tightly controlled and delivers consistent high-quality cells, we’re going to get the answer.”
Homegrown Meds
Cell therapies can come from a couple of different sources. The two most common types of stem cell transplants for cell therapies are autologous and allogeneic. With an autologous transplant, the patient’s own cells are removed, expanded, modified for a therapeutic purpose – finding and attacking cancer, for example. In an allogeneic transplant, the patient receives cells – say, bone marrow or peripheral blood stem cells – from a matching donor, typically a sibling.
“Cells can do many things that a single molecule can’t do,” Roy says. “A cell is a complex entity – a living and breathing entity. They can multiply inside the body, attack and kill certain other cells, like cancer, change the behavior of other cells, like immune cells. These can be extremely powerful drugs. If not harnessed properly, they can be deleterious to a patient as well.”
The side effects with the Novartis drug almost killed Emily Whitehead. These include high fevers, low blood pressure, seizures, liver abnormalities, and heart irregularities. The company and clinicians have developed strategies to manage and minimize the risks.
In the end, for the great majority of patients in the study, the reward was well worth the risks. “Our daughter was going to die, and now she leads a normal life,” Emily’s father, Tom Whitehead, told the FDA panel that endorsed the therapy.
Wilbur Lam is a physician – a hemotologist/oncologist – as well as a researcher in the Petit Institute. He’s seen what happens when standard therapies fail and much prefers having an alternative.
“Cell therapies are the next generation of therapeutics. They offer hope,” says Lam, associate professor in the Coulter Department, and a pediatrician with Children’s Healthcare of Atlanta and the Emory School of Medicine.
His lab has developed a technology in which the patient’s own platelets – the cells that control blood clotting – can be used as a delivery system for drugs. “When it gets to a bleed, it can release its cargo, because the platelet is fine tuned to react to the environment,” Lam says.
It’s a treatment that can be used for patients with hemophilia, or patients who have experienced trauma and are bleeding. “We can also fine tune this system to go in the opposite direction, use it to deliver anti-clotting medications for patients who have heart attacks or strokes,” Lam says. “All of which is enabled by the patient’s own platelets, which act as the brain and muscle, releasing the drug only where it needs to be.”
Petit Institute researcher Melissa Kemp has some personal reasons for her interest and work in cell therapy research, which is based in computational systems biology. Her lab is interested in how intracellular and extracellular environments control the transmission of cellular information, studying living systems using engineering and computational tools, basically looking at complex protein networks the way an electrical engineer might look at a power grid.
“We want to understand how these things are connected together – if you have a failure at one spot, how does that propagate and cause a blackout in another location,” says Kemp, associate professor in the Coulter Department, whose family medical history includes conditions that cell therapies would address.
“Some of the target applications that Georgia Tech researchers have in mind include cardiovascular disease, osteoarthritis, cancer – all of which run in my family,” says Kemp, whose father is a cancer survivor. “So, I’m really excited about the potential of these end applications. The exciting aspect about cellular manufacturing is the ability to really revolutionize medicine in this century.”
Media Contact
Jerry Grillo
Communications Officer II
Parker H. Petit Institute for
Bioengineering and Bioscience
Keywords
Latest BME News
Jo honored for his impact on science and mentorship
The department rises to the top in biomedical engineering programs for undergraduate education.
Commercialization program in Coulter BME announces project teams who will receive support to get their research to market.
Courses in the Wallace H. Coulter Department of Biomedical Engineering are being reformatted to incorporate AI and machine learning so students are prepared for a data-driven biotech sector.
Influenced by her mother's journey in engineering, Sriya Surapaneni hopes to inspire other young women in the field.
Coulter BME Professor Earns Tenure, Eyes Future of Innovation in Health and Medicine
The grant will fund the development of cutting-edge technology that could detect colorectal cancer through a simple breath test
The surgical support device landed Coulter BME its 4th consecutive win for the College of Engineering competition.