The newest class of graduates from the Master of Biomedical Innovation and Development program presented new devices to help with patient care, emergency medicine, and chronic debilitating illnesses during their final project pitches Aug. 1.
The presentations resembled just the kind of pitch a startup company might give to potential investors — a fitting capstone to the intensive one-year master’s program in the Wallace H. Coulter Department of Biomedical Engineering focused preparing a new generation of leaders in medical device innovation and commercialization.
“We chose that focus very carefully and have stuck to it through the years,” MBID Program Director Sathya Gourisankar told the graduates, who assembled in the Krone Engineered Biosystems Building to present their final projects. “But also, we want to contribute to the placement and advancement of the medical device industry in the Southeast, particularly in Atlanta.”
In its ninth year, the program has now produced 234 graduates, and the 2021-22 class enjoyed the first in-person graduation in two years. Split into five teams, the students operated very much like medical device startups, building a bench-to-bedside pathway to product commercialization.
A team developed a simple chemical-based heating device to help trauma patients with hypothermia in the critical early minutes of care. Students designed a better stent to help avoid urinary tract infections and a simple wearable to help Parkinson’s patients get moving again after freezing-of-gait episodes.
One device helps with cerebrospinal fluid draining for patients with intracranial hemorrhaging, while one team developed a simple system to allow nurses to safely and gently turn immobile critical care patients by themselves.
It’s all part of Gourisankar’s playbook to train students in every aspect of product development: They identify unmet clinical needs and develop a device, studying the market viability and regulatory environment, pitching the product, and learning how to raise capital.
“Our graduates experience a broad overview and familiarity with the development process – the building blocks, from concept to commercialization,” said Gourisankar, who developed the program that has now produced 234 graduates.
Some have applied what they’ve learned to carry on with their MBID projects and commercialize their device or to pursue other entrepreneurial possibilities. Some are clinicians looking to expand their entrepreneurial skillsets. And some have entered the workforce as senior-level employees in the medical device industry. All are prepared to be the furture leaders in the industry, Gourisankar said.
Here’s a rundown of the MBID projects from the class of 2021-2022:
Aurora Nova
Team: Alec Mills, Cassandra Tom, Arthan Bhatt, Chen Zhang, Neha Potdar, Obaid Hussaini, Taylor Farnan.
Problem: Upper urinary tract obstructions can develop into kidney failure and sepsis, making them deadly conditions if not treated effectively and quickly. The current preferred method for restoring drainage, ureteral stents, preserves normal urinary function. But they have some complications that can cause urinary tract infections, and in about 80 percent of patients, pain.
Solution: A better ureteral stent to provide better value for hospitals, a treatment advantage for physicians, and comfort for patients. Design changes reduce patient discomfort and the number of repeat visits to the doctor, while the use of proven biomaterials reduces the rate of infection and sepsis.
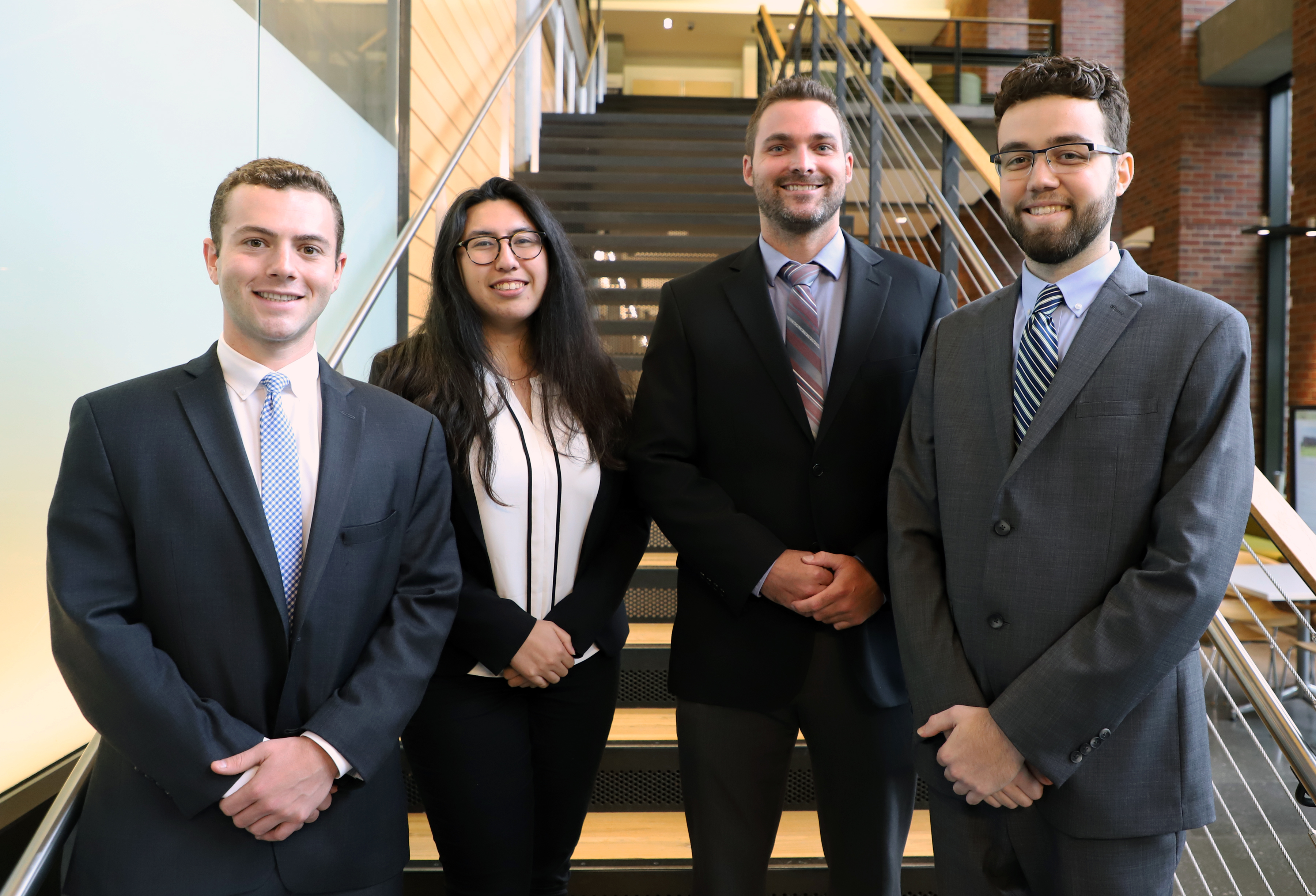
Core Biomed
Team: Grant Berliner, Trevor Pearce, Jen Ternullo, Bryce Huff, Jose Lopez, Will Esseks
Problem: More than 400,000 patients in the U.S. are admitted each year to trauma centers while suffering from prehospital hypothermia, a sometimes-deadly condition caused by severe blood loss. These patients also have a one-day longer length of stay in the hospital, compared to patients with similar injuries, and a greater chance of needing a blood transfusion, which costs U.S. trauma care systems $4.95 billion per year.
Solution: The MVP, an easy-to-use, disposable, adhesive heating device developed after interviews with emergency medical personnel. The MVP is a chemically heated pad designed to quickly supply at least an hour of local heat after being activated, buying precious time for trauma patients.
Emergent Tech
Team: Deena Bhula, Courtney Mobbs, Anirudh Viswanathan, Ananya Kamath, Soumya Samantaray and Henry Fawole
Problem: Many patients in the Intensive Care Unit are sedated or immobile. Whenever a nurse needs to change sheets, clean the patient, or provide other care, the patient must be manually turned, a difficult task that can require several staff members. The challenge is repositioning immobile patients in a way that reduces time, the number of staff required, and the risk of injury to healthcare providers and patients.
Solution: Kratos, a simple, a somewhat low-tech device consisting of four basic parts: C-clamps, carabiners, straps, and an automatic winch. The repositioning system, which can be deployed by one caregiver to rotate the patient from a supine to a stable lateral position, makes the process easier and safer, and helps maximize hospital staff time during a national nursing shortage.
Medicure
Team: Aadil Vora, Alberto Castro, Elliott Bauer, Grayson Goss Kinjal Mutha, Sarika Karri, Ramesh Arvind S.
Problem: Intraventricular hemorrhage is the most severe form of intracranial hemorrhage, already the deadliest form of stroke. The standard of care is a shunt that drains out cerebral spinal fluid (CSF). However, clotting and occlusions often occur that prohibit proper drainage and can lead to severe brain damage or death.
Solution: A device called ReVentri. The device uses rotating impellers to break down clotting and facilitate different rates of drainage, using a software interface to control impeller speed. The goal is to create a proactive, hands-free approach to managing CSF drainage so clinicians can focus on other aspects of the patient’s critical care.
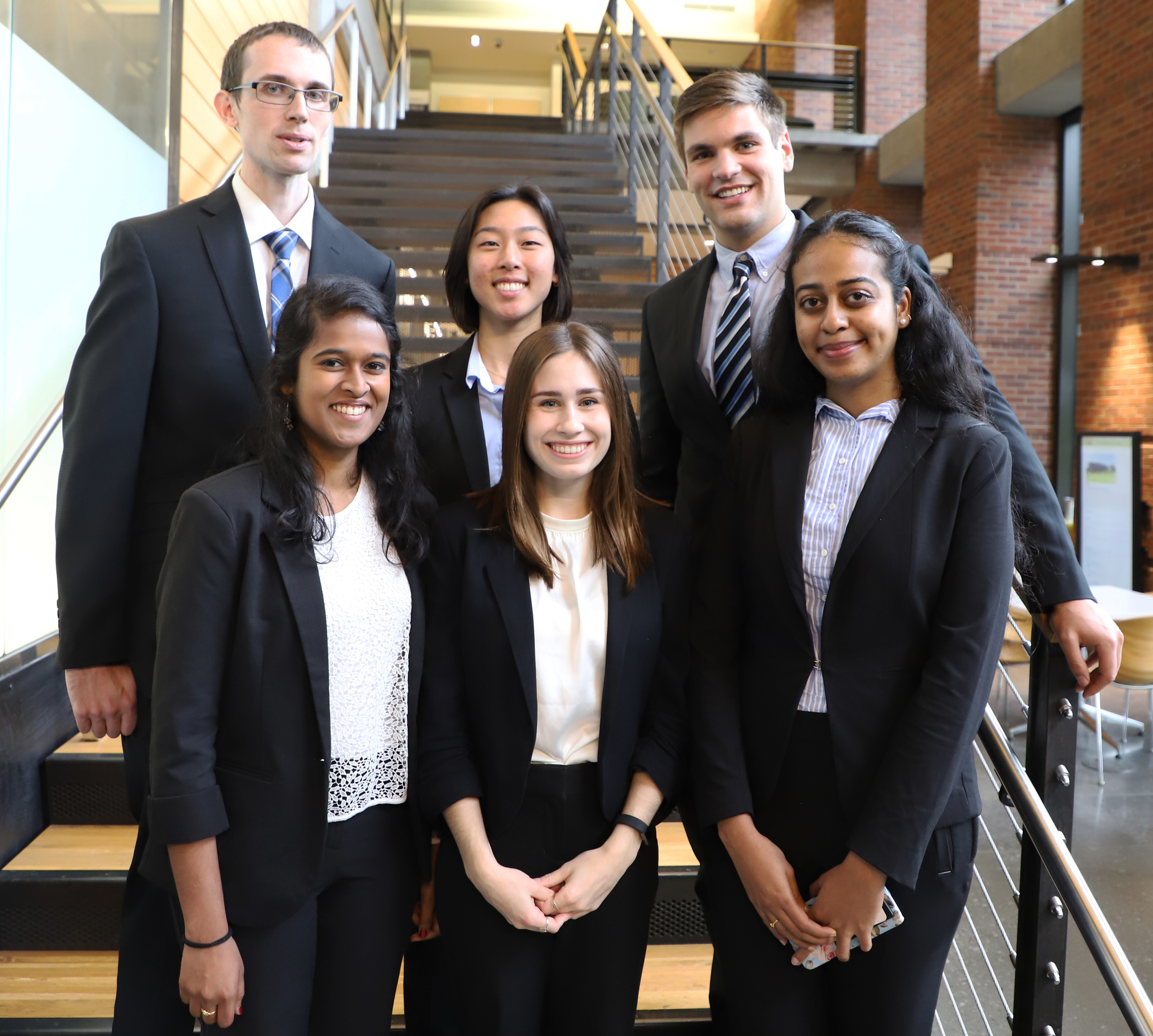
OSTEON (Original Solutions Team Envisioning Orthopedic Needs)
Team: Michael Bennett, Lucia Coco, Maggie Hsieh, Christian Logarbo, Ramya Natarajan, Deepika Suresh
Problem: Parkinson’s disease patients struggle with gait degradation and freezing of gait, symptoms that contribute to dangerous falls. These patient falls represent a large portion of what is estimated to be a $101 billion cost to the healthcare system by 2030. The team set out to develop a way to prevent falls in Parkinson’s patients by helping them restore their balance.
Solution: A wearable device that provides long-term gait improvement via electrical muscle stimulation, and short-term fall prevention via vibratory cueing. Sensors track patient movements, and an algorithm detects a freezing of gait episode. Detection cues a vibratory pulse to break the patient out of the episode.
Latest BME News
Jo honored for his impact on science and mentorship
The department rises to the top in biomedical engineering programs for undergraduate education.
Commercialization program in Coulter BME announces project teams who will receive support to get their research to market.
Courses in the Wallace H. Coulter Department of Biomedical Engineering are being reformatted to incorporate AI and machine learning so students are prepared for a data-driven biotech sector.
Influenced by her mother's journey in engineering, Sriya Surapaneni hopes to inspire other young women in the field.
Coulter BME Professor Earns Tenure, Eyes Future of Innovation in Health and Medicine
The grant will fund the development of cutting-edge technology that could detect colorectal cancer through a simple breath test
The surgical support device landed Coulter BME its 4th consecutive win for the College of Engineering competition.