Two senior design teams publish reports on their brain-related projects in academic journals
Increasingly, a senior design project isn’t just a senior design project.
Intended as the “capstone” to students’ time in the Wallace H. Coulter Department of Biomedical Engineering, these projects often become presentations to outside groups, posters at professional conferences, or even fledgling startups.
Now, they’re also resulting in published research papers in academic journals.
Two different Coulter BME Capstone Design teams published papers in recent weeks that grew from their work on a problem presented by an outside project sponsor — even though all of the team members have since graduated and moved on to internships, jobs, and graduate school. One study describes a surgical simulation tool for training neurosurgeons or preoperative planning for brain surgery. The other paper documents, perhaps for the first time, the potential harm to the brains of U.S. Army Ranger mortarmen from repeatedly firing their weapons systems.
The Cumulative Effects of Low-Level Blasts
Army Ranger mortarmen test fire a 120 mm mortar at Fort Benning in Columbus, Georgia. A team of Coulter Department students has published a study in the journal Military Medicine documenting the potential brain injuries for mortarmen caused by repeated low-level blasts caused by firing their weapons systems. It's perhaps the first time the actual blast pressures have been reported and points to "a concerning health risk for mortarmen,” the team wrote. (Photo Courtesy: Project Halo team)
The initial charge to Jessica McElrath, Brady Muñoz (née Bove), Jordyn Sak, Grace Trimpe, and Julia Woodall was broad: mitigate mild traumatic brain injury (TBI) among Army Rangers. It wasn’t until they dug in and started talking to Rangers with TBI symptoms that they zeroed in on mortarmen.
“There are so many mortarmen who are talking about having headaches, memory issues, and all these different symptoms related to concussion and mild traumatic brain injury, yet there are very few who are actually diagnosed, let alone treated,” Sak said. “They don't have a blast event to account for those symptoms. And it became clear it's not one big blast event — they're exposed to hundreds of small blast events repeatedly over time, and that's contributing to a problem.”
The team combined data about symptoms reported by mortarmen with their pupils’ reflexive response to light, a recognized measure of changes in brain function. They also measured the actual pressure produced by firing the mortars, known as blast overpressure. Their findings, published in Military Medicine, suggested “a concerning health risk for mortarmen” and recommended “immediate action” — namely, “[b]ehavioral changes like ducking and standing farther from the mortar when firing” as well as daily safety thresholds and firing limits during training.
The Project Halo team worked with Army Rangers at Fort Benning in Columbus, Georgia, to collect data about the blast overpressure produced by firing mortars. Their Capstone project goal was to create a blast attenuation device, but the team said their paper in Military Medicine has the potential to have much more impact for soldiers. (Photo Courtesy: Project Halo team)
McElrath pointed to other weapons systems with established daily limits, like a Carl Gustaf recoilless rifle, that allow soldiers to fire just two rounds per day. No similar standard exists for mortarmen.
“The guys we were talking to would go on their deployment or during training and shoot upwards of 100 [mortar] rounds per day,” McElrath said. “We found they were exposed to similar pressure values as to what these recoilless rifles were giving off, and there's no firing limits. There's nobody telling them to stop or what that's doing to their brain.”
Woodall likened it to the fatigue engineers measure for other materials: “If you keep cyclically loading the brain with these lower pressures than you get from these other weapon systems, there's still this cumulative damage occurring, but it wasn't really recognized. For me, that's why I was really motivated to pursue publishing the paper.”
McElrath said one of the officers they worked with suggested their data could be useful in justifying changes to training, such as switching to expensive mortar simulators that don’t produce the harmful blast overpressure. Sak suggested their data could help establish treatment options through the Veterans Administration health system for former mortarmen.
“There are a few other papers out there, not with mortar systems, but others that are starting to credit how cumulative blast exposure is really detrimental to brain health,” Woodall said. “We think this is adding to the wave of those papers that are really going to make a paradigm shift, hopefully, in how the military views preventative measures as a way to safeguard mortarmen and military service members’ health.”
Practicing Brain Surgery Outside the OR
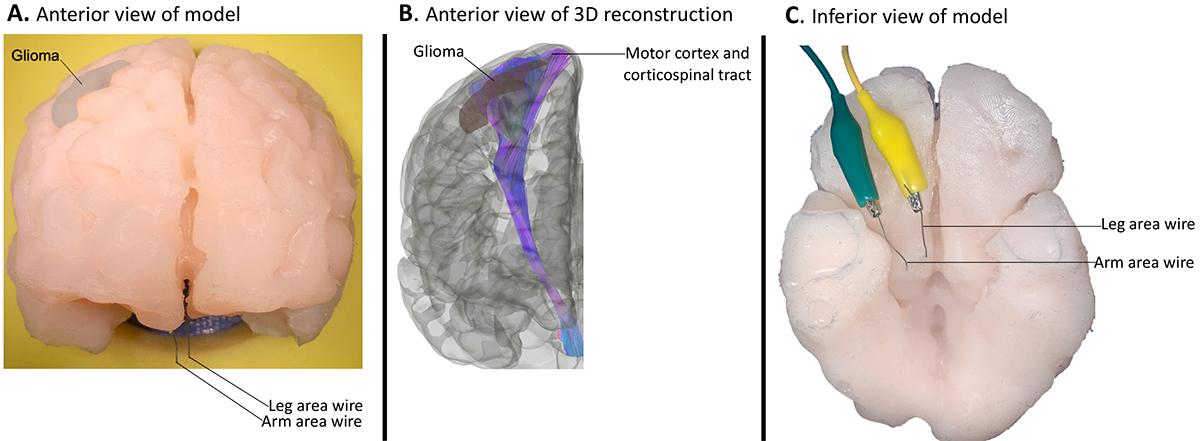
This illustration shows the brain mapping simulator designed by the Brainy Bunch team and reported in the journal Operative Neurosurgery. The simulator is patient-specific, anatomically accurate, and electrically responsive. The middle image is a 3D reconstruction of a magnetic resonance scan that the team used to guide placement of the wires in their model. (Illustration Courtesy: The Brainy Bunch)
Brain function also was core to the work of Faith Colaguori, Rebecca Forry, Maité Marin-Mera, and Megan McDonnell.
Working with the Mayo Clinic, their charge was to develop a training device to help residents and trainees practice brain surgery techniques outside of the operating room. They 3D-printed a mold to create a patient-specific, anatomically accurate, and electrically responsive brain model that simulates the mapping that surgeons do to identify functional brain areas during surgery.
In a study published in Operative Neurosurgery, the team and their co-authors called the model “the first of its kind as a functional anatomic model that allows stimulation of brain tracts not available in even the best cadaveric specimens.”
Though the idea was to help with training, it quickly became clear the tool could be useful for experienced neurosurgeons too, McDonnell said.
“As we went through the project, it also took on this role as a preoperative planning tool that could be used by neurosurgeons of any skill level,” she said. “The doctor could basically print out a version of the case that they're about to perform and use it as a practicing tool before they're operating on the live patient.”
The team built their proof-of-concept model using anonymized patient brain scans, and they embedded wires to simulate the electrical properties of brain tissue. It adds to the work their sponsor at Mayo, Alfredo Quiñones-Hinojosa, has been doing on surgical modeling and planning tools.
“It is really on the forefront of modeling the neural pathways and being able to replicate this surgical scenario outside of the operating room, because cadaveric tissue cannot create this kind of environment — you can't practice brain mapping on cadaveric tissue,” Marin-Mera said. “Being able to do that outside of the operating room — in an environment where there's not a patient on the table and where the surgeon is trying to teach and do the surgery at the same time — is really important. Mayo Clinic definitely strives to create these novel ways of teaching.”
As the team developed their model, they tested it with nearly three dozen surgeons, who told them it was key for the model to accurately mimic brain anatomy as well as the tactile and electrical stimulation feedback of surgery. Nearly all of them found the model to be useful for training.
“I'm really interested in translational research and trying to bridge that divide between preclinical work in the lab and things that can actually be applied in the hospital. This project was a really great way to explore that,” Colaguori said. “We had the opportunity to work with these clinicians, who are some of the world's experts in this type of surgery, and combine the skills that we learned in our engineering degree with these pure scientific perspectives that they had. Together, we were able to make a really transformative device that bridged both disciplines.”
Related Links
- "Three-Dimensionally Printed Surgical Simulation Tool for Brain Mapping Trainin…
- "Repetitive Low-level Blast Exposure and Neurocognitive Effects in Army Ranger …
- Coulter BME Capstone Design
- Fall 2020 Capstone: The Brainy Bunch
- Fall 2020 Capstone: Project Halo
- National Security Innovation Network X-Force Fellowship
Latest BME News
Jo honored for his impact on science and mentorship
The department rises to the top in biomedical engineering programs for undergraduate education.
Commercialization program in Coulter BME announces project teams who will receive support to get their research to market.
Courses in the Wallace H. Coulter Department of Biomedical Engineering are being reformatted to incorporate AI and machine learning so students are prepared for a data-driven biotech sector.
Influenced by her mother's journey in engineering, Sriya Surapaneni hopes to inspire other young women in the field.
Coulter BME Professor Earns Tenure, Eyes Future of Innovation in Health and Medicine
The grant will fund the development of cutting-edge technology that could detect colorectal cancer through a simple breath test
The surgical support device landed Coulter BME its 4th consecutive win for the College of Engineering competition.