The one-year Master in Biomedical Innovation and Development (MBID) program was created in 2013 by the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory to fill a market need for innovative professionals thoroughly trained at the intersection of biomedical device engineering, healthcare, and business development.
“The MBID curriculum and training are founded on the twin pillars of real world exposure and state-of-the-art industry practices,” said Sathya Gourisankar, director of the MBID master’s program, who designed the program’s curriculum and has more than 30 years of product development experience in the medical device industry.
According to Gourisankar, “this kind of [real-world] focus has enabled the program to graduate students capable of working across a variety of roles—a fact that has been well accepted by the medical device industry, resulting in repeat hiring and requests for hiring of future program graduates from industry leaders as well as start-ups. The longer-term objective of the program is to train the next generation of industry leaders for medical device development and commercialization.”
This year, the program graduated its largest class of MBID students. Final presentations were delivered last week in a large auditorium at Georgia Tech’s Scheller School of Business, where six MBID teams each presented innovative and new medical devices that could improve healthcare and lower costs. Prior to selecting a medical problem to solve, each team has to research the market viability (including a patent search) of their proposed medical device.
“The MBID program provided an excellent basis and overview for the medical device industry as a whole. Up until this point, my undergraduate education only gave me some creative skills, technical abilities, and a baseline understanding of the regulatory process. The MBID program brought that understanding much deeper, as well as introduced whole areas of the medical device industry that I did not even realize were crucial to the development of a medical instrument,” said Jack Novak. “As a future physician, I know this will provide me with a crucial understanding of the development and process of approval behind the devices I use.”
Yuting Bai, a student in this year’s graduating class said, “the MBID program is a great opportunity to explore roles and career paths in the medical device industry. Apart from this, the 12 month long team project in product development has truly enhanced my leadership skills, communication with external experts and internal teammates, as well as dealing with real-life team conflicts as we developed and designed our new, innovative technology.”
“The program has done a great job teaching us how to take a medical device from bench to bedside,” remarked MBID student David Shumate. “Our team has filed a provisional patent on the illuminating catheter we developed, and we will be the owners and inventors after graduating from the [MBID] program!”
Novack, who has already been accepted into medical school, delivered these parting remarks, “an absolute highlight of the MBID program is the actual device development you do in small teams within your class. This allows you to apply what you are learning in the classroom by taking a medical device that you prototype and test from bench to theoretical bedside.
“My team’s project was a therapy for osteoporosis that would allow elderly patients in our target group to preemptively increase their bone density prior to surgery,” Novack continued. “My team was able to test our device on bone cells and found a significant increase in gene expression after treatment, which is an excellent indicator of the feasibility of the actual device. We hope to continue working on it even as our teams goes separate ways in the workforce.”
Below is this year’s complete list of each MBID student team, project area, team name, team members, and project description:
[CARDIO] Team: BraveHearts Team Members: Catriona Tarto, Ashish Joishy, Tanay Garg, Jacob Rodenbusch, Divya Raghavi, and Deepthi Badarinath Clinical Mentors: Gautam Kumar, M.D. and Ravi Rajani, M.D. Project Description: The BraveHearts Team developed Venux, an endovascularly implanted stent with a unique geometrical design, to treat patients suffering from Chronic Venous Insufficiency (CVI) with the presence of Deep Venous Reflux (DVR). The gold standard treatment option is surgical popliteal vein banding, which is not ideal. The procedure has a higher risk of complications and is only offered once the disorder has progressed and significantly increased in severity. Our solution is minimally invasive, requiring only a simple Cath Lab procedure, and could potentially treat patients before development of venous ulcers.
[OB-GYN] Team: FemMed Team Members: Yuting Bai, Madelyn Golding, Yeasul Kim, Kevin Nguyen, Samiksha, and Andy Ung Clinical Mentor: Robert Kelley, D.O., MBA.
Project Description: The FemMed team developed a technology, CalipHER, capable of accurately measuring the vaginal canal both quantitatively and qualitatively in order to aid in the correct selection and prescription of the nonsurgical pessary device for treatment of pelvic organ prolapse (POP) in adult women. Current mismeasurement and subsequent incorrect prescription of the pessary device leads to many problems and has a high failure rate of 42%. This team identified a need to improve the use of the pessary as an effective treatment for POP by allowing measurements to be performed in the office setting, by the OB/GYN, via an electromechanical vaginal insert that gives the doctor real-time feedback to aid in their decision making. CalipHER will not only redue problems related to current pessary device use, but upon adopting CalipHER, hospitals and OB/GYN private practices could increase their margins and prevent negative revenues (since CalipHER can prevent secondary injuries and unnecessary surgeries from occurring). FemMed is working with OB/GYNs and specialized urogynecologists in Atlanta to streamline the usage of the device and reduce the burden of current pessary usage and failure rates on the healthcare system.
[UROLOGY] Team: Health Pass Team Members: Jack Blumeyer, Shashwat Hora, Jon Luedtke, Pranav Padmanabha, David Shumate Clinical Mentors: Spencer Kozinn, M.D.; Raymond Pak, M.D., and Jaime Wong, M.D. Project Description: The Health Pass team developed the FoLED Catheter which is a device that has been developed for use in prostate cancer cases requiring radical prostatectomies. The device introduces a novel method of locating the bladder neck junction between the bladder and the prostate, improving on a crucial step in prostatectomy surgeries. This cuts down on procedural time reducing cost, and allows for a more efficient procedure with better outcomes.
[ICU] Team: I-CUra Tech Team Members: Jennifer Arkin, Dipro Chakraborty, Cristina Ibanez, Ben Myers, Shraddha Patel, and Jaclyn Sider Clinical Mentor: Maxwell Weinmann, M.D.
Project Description: In the U.S., 2.5 million ICU patients develop pressure ulcers costing more than $15 billion a year. The I-CUra team developed SacralSense, a pressure ulcer preventative hydrofoam dressing that redistributes pressure across the sacrum and measures interface pressure and bioimpedance ICU patients. The SacralSense system is designed as a stand-alone technology to replace current sacral hydrofoam dressings, worn by the majority of ICU patients, for prevention of pressure ulcer onset and progression on the sacrum. Nurses will apply and monitor the device, which will provide a more quantifiable prevention tool than current sacral hydrofoam dressings that only redistribute pressure. SacralSense also consists of a user interface (UI) that alerts nurses when a patient’s pressure or bioimpedance levels are out of normal range. This will alert the nurse that further preventative measures are needed to prevent onset or progression of a pressure ulcer on the sacrum. The UI will also hold patient information, including current preventative measures and treatments applied, relevant medical information, and trends of pressure and bioimpedance readings over time. The system improves patient quality of life, reduces length of stay, and reduces healthcare costs for both patients and hospitals.
[ORTHO] Team: OrthoJackets Team Members: Earl Bender, Hunter Hatcher, Connie Leung, Jack Novack, Aken Sanghavi, Kayla Walley. Clinical Mentor: Dheera Ananthakrishnan, M.D.
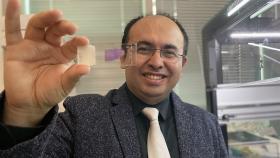
Project Description: 60 million people are projected to have osteoporosis in the United States by 2020, in the United States alone. A large portion of these patients have underlying condition which require spinal surgery however, due to low bone mass in the spine, there is a much higher complication rate associated with these procedures and around 20% of osteoporotic patients are turned away, unable to get the surgery they need. To address this urgent clinical need, the OrthoJackets team developed V.I.B.E.: a pre-surgical targeted vibrational therapy designed to increase bone density in osteoporotic and osteopenic patients. V.I.B.E. is a wearable device, which delivers mechanical vibrations directly to the spine. OrthoJackets has performed multiple cell studies which have shown that the vibrations induce proliferation of osteoblasts and lead to an increase in bone mass. This allows users to undergo previously inaccessible elective surgery, significantly reducing pain and discomfort, and greatly increasing overall quality of life.
[EMS/Pre-hospital] Team: Vocatus Team Members: Chandra Yarlagadda, Nicholes Hillborn, Abinaya Selvakumar, Lucia Lopez, Eric Oliver, Nishtha Bhan Clinical Mentor: Lekshmi Kumar, M.D. Project Description: Vocatus developed Dynamore, a truncal and junctional hemorrhage controlling device. Hemorrhages are the second largest cause of death due to trauma, behind only traumatic brain injuries. There are approximately 50,000 deaths each year due to traumatic hemorrhages, with 70-80% of these deaths occurring from wounds in the truncal and junctional area where tourniquets cannot be applied. In the military setting, 72% of all preventable deaths in the field are due to bleeding from truncal and junctional regions. Vocatus has identified the need to control truncal and junctional external hemorrhages in an emergency environment to reduce blood loss and increase the patient survival rate. Truncal and junctional hemorrhages are one of the leading causes of preventable deaths in the US civilian and military market. While there are currently products that attempt to solve these problems they are often lacking in ease of use, efficacy, and cost.
Media Contact
Walter Rich
Keywords
Latest BME News
Jo honored for his impact on science and mentorship
The department rises to the top in biomedical engineering programs for undergraduate education.
Commercialization program in Coulter BME announces project teams who will receive support to get their research to market.
Courses in the Wallace H. Coulter Department of Biomedical Engineering are being reformatted to incorporate AI and machine learning so students are prepared for a data-driven biotech sector.
Influenced by her mother's journey in engineering, Sriya Surapaneni hopes to inspire other young women in the field.
Coulter BME Professor Earns Tenure, Eyes Future of Innovation in Health and Medicine
The grant will fund the development of cutting-edge technology that could detect colorectal cancer through a simple breath test
The surgical support device landed Coulter BME its 4th consecutive win for the College of Engineering competition.